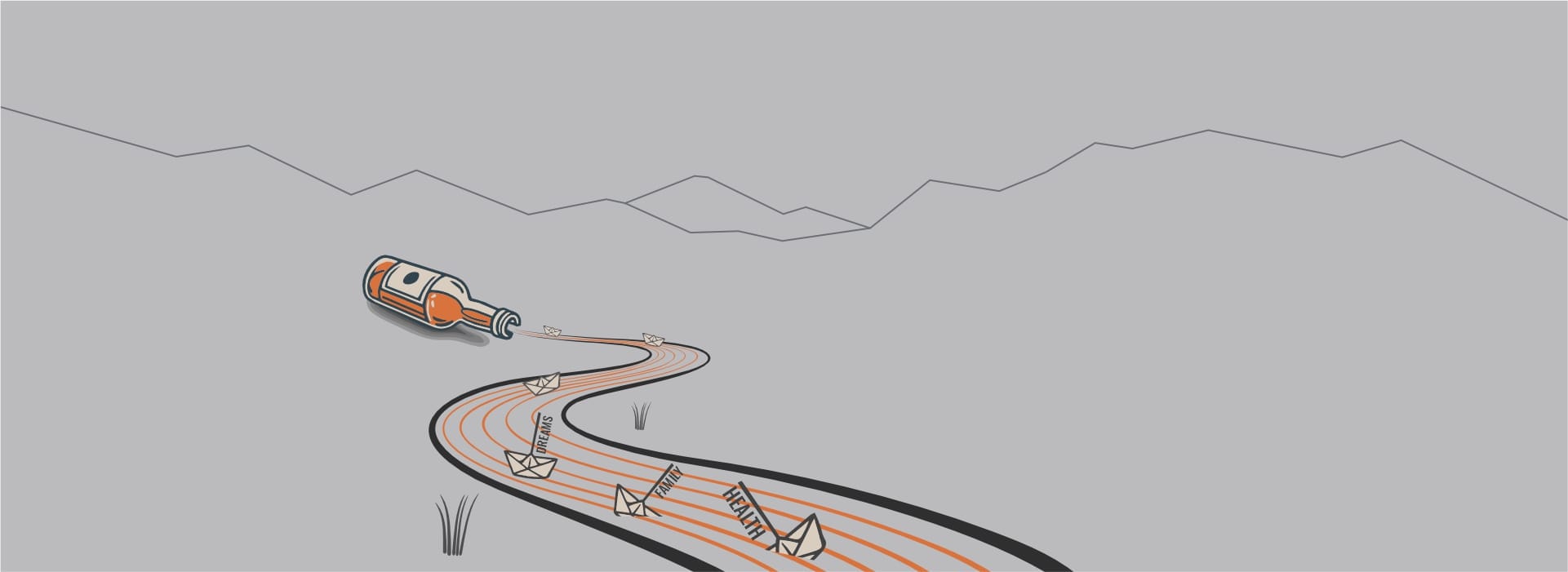
Understanding the Causes of Alcoholism in Older Adults
Unveiling the Link between Loneliness and Alcoholism

The intricacies of human emotions and social structures reveal a poignant vulnerability among older adults, predominantly through the lens of loneliness. Empirical data underscores a distressing correlation between social isolation and the propensity toward alcohol dependency. Loneliness, described by psychologists as the distressing experience that occurs when one's social needs are not met by the quantity or quality of their social relationships, can significantly exacerbate the risk factors associated with alcoholism. This psychological state often serves as fertile ground for turning to alcohol as a coping mechanism, creating a cycle of dependency difficult to break without intervention.
Research delineates that the absence of social interactions can potentiate the release of stress hormones in the body, amplifying feelings of depression and anxiety, conditions closely linked to increased alcohol consumption in geriatric demographics. The neurobiological pathways involved suggest a complex mechanism wherein the reward systems of the brain may become more susceptible to the effects of alcohol, making older adults more vulnerable to its sedative properties. This biochemical perspective provides a crucial insight into the physiological underpinnings that foster alcoholism in response to loneliness.
| Aspect | Description |
|---|---|
| Loneliness and Alcoholism | Direct correlation between increased feelings of loneliness and higher alcohol consumption among older adults. |
| Neurobiological Pathways | Evidence suggests loneliness affects the brain's reward system, increasing susceptibility to alcohol's effects. |
| Role of Social Structures | Weak or nonexistent social connections increase risks of alcohol dependency due to lack of emotional support. |
| Psychological Impact | Stress, depression, and anxiety from loneliness can lead to self-medication with alcohol. |
With a comprehensive understanding of the nexus between loneliness and alcoholism in older adults, it's imperative to foster a societal and medical approach that encompasses not only the physical but also the emotional and social health of this demographic. Strategies aimed at increasing social interaction and support systems could mitigate the impact of loneliness, thereby indirectly reducing the propensity for alcoholism. Hence, addressing the epidemic of loneliness among the elderly is not just an issue of social well-being but a vital component in curbing the rise of alcohol dependency in this vulnerable population.
The Hidden Influence of Chronic Pain Management
Chronic pain, a pervasive affliction among the elderly, often necessitates long-term management strategies, sadly intertwining with increased alcohol consumption for some. As the body ages, susceptibility to conditions like arthritis, neuropathy, and osteoporosis escalates, frequently leading individuals down a path seeking relief beyond prescription medication. The transition towards using alcohol as a coping mechanism arises subtly, often justified by its initial efficacy in dulling pain. However, this temporary solace masks a perilous slope toward dependency. The physiology of older adults complicates this narrative further. With age, the body's ability to metabolize alcohol diminishes, enhancing its sedative effects, yet simultaneously increasing vulnerability to its adverse consequences. Therefore, when alcohol is employed as a supplementary pain management tool, it unwittingly contributes to the exacerbation of alcoholism in older people.
This intertwined relationship between chronic pain management and the risk of alcoholism is compounded by the often-undervalued importance of comprehensive pain assessment and tailored pain management strategies in elderly care protocols. The medical community stresses the significance of distinguishing between treating pain and inadvertently facilitating a dependency on alcohol. Holistic approaches that encompass physical rehabilitation, psychological support, and, when necessary, appropriate medication management, are pivotal. Such strategies not only address the root cause of the pain but also safeguard against the pitfall of alcohol misuse.
The intricacies of this challenge demand a multi-disciplinary approach to healthcare, intertwining pharmacological interventions with psycho-social support. Raising awareness among healthcare professionals regarding the risks of alcohol misuse in the context of pain management is crucial. Equally important is educating older adults and their caregivers about the potential dangers of self-medicating with alcohol. By enhancing understanding and vigilance around this issue, it becomes possible to mitigate the risks associated with alcoholism in older people and improve their overall quality of life. This concerted effort can pave the way for a more informed, empathetic, and effective approach to managing chronic pain in the elderly, recognizing the fine line between relief and risk.
Retiring from Work: a Gateway to Drinking?
Transitioning into retirement marks a significant change in an individual's life, bringing about a complex mix of emotions and adjustments. For many, this phase signals freedom and the opportunity to explore new horites. Yet, it can also be a period of profound loss—loss of identity, routine, and social interactions. The void left by the absence of work can lead individuals to seek solace in various ways, with alcohol becoming a seemingly easy escape for some. This shift towards increased alcohol consumption can be subtle, initially perceived as harmless relaxation or celebration of retirement. However, the gradual increase in dependency often goes unnoticed until it escalates into a more severe condition of alcoholism in older people.
Psychological research sheds light on how the structure and routine provided by work serve as critical components in an individual's mental health. Without the daily demands of a job, retirees might find themselves confronting feelings of uselessness and purposelessness—emotions that significantly contribute to mental health decline. Alcohol, in this context, can become a coping mechanism to numb these discomforting feelings. Moreover, the social isolation that can accompany retirement exacerbates this dynamic, as older adults find fewer opportunities for social engagement outside the workplace. The lack of a supportive social network makes the slide into alcohol misuse more likely, underlining the importance of understanding this transition's psychological impacts.
Physiologically, older adults experience a decline in the body's ability to process alcohol, making the effects more potent and damaging even at lower consumption levels. Despite this, there may be a lack of awareness or denial about the increased risks associated with alcohol consumption in this stage of life. This underestimation can lead to the development of alcoholism, with its consequential health implications being more severe in the older population. The interaction between alcohol and medications, which are more likely to be taken by older adults for various health issues, poses additional risks, further complicating the situation.
To address these challenges, it is imperative that healthcare professionals, families, and communities promote healthier coping mechanisms and social engagement opportunities for retirees. Holistic approaches that consider the psychological, social, and physiological changes associated with retirement are essential in preventing and treating alcoholism in older people. Providing targeted support and resources can help mitigate the risks, ensuring that retirement becomes a period of growth and positive transformation rather than a gateway to unhealthy habits.
The Unseen Role of Bereavement and Loss
The profound impact of bereavement and loss on older adults cannot be overstated, often serving as a catalyst for increased alcohol consumption. The grieving process brings about a multitude of complex emotions, ranging from sorrow and anger to guilt and loneliness, leading some seniors to turn to alcohol as a form of solace. Scientific studies have shown that the acute stress related to loss can exacerbate existing mental health conditions or usher in new psychological challenges, making alcohol an appealing, albeit harmful, coping mechanism. This susceptibility is particularly pronounced among this demographic, who may find themselves more isolated following the death of a spouse, close friend, or sibling, further entrenching the alcohol dependency cycle.
Moreover, the physiological effects of aging interact with alcohol in ways that can heighten its impact on mood and cognitive function, making alcoholism in older people a uniquely complex issue. Reduced metabolic rates mean alcohol remains in an older adult's system for longer periods, increasing the likelihood of dependence and exacerbating the psychological toll of grief. Additionally, the social stigma attached to expressing vulnerability or seeking help for emotional pain often deters seniors from accessing the necessary support services, leaving alcohol as one of the few perceived outlets for their anguish.
To effectively address this challenge, it is essential to promote a broader understanding of the grief process within this age group and the dangerous role alcohol can play in it. Providing targeted support services that address the specific needs of grieving older adults, including counseling and social support networks, can play a crucial role in preventing the onset of alcohol misuse. Equally important is the need for healthcare providers to be vigilant in recognizing the signs of alcohol dependency in their elderly patients, particularly following significant life losses, to intervene before the problem escalates. Through a combination of education, support, and proactive health care measures, it is possible to mitigate the risk of alcoholism triggered by bereavement and loss in the elderly population.
Identifying Medication Interactions and Alcohol Misuse
The intersection of pharmacological therapy and alcohol consumption presents a complex arena of challenges for older individuals. Polypharmacy, a common circumstance among the senior population, increases the risk of adverse drug reactions, a situation further complicated when alcohol is introduced into the equation. Ethanol interacts with medications through various mechanisms, including altering their metabolism and bioavailability or exacerbating their sedative effects. These interactions can lead to diminished therapeutic efficacy or heightened toxicity. For instance, alcohol can significantly increase the sedative effects of psychotropics, posing serious risks such as respiratory depression or cognitive impairment. Furthermore, ethanol's ability to interfere with the metabolism of medications like warfarin can lead to either subtherapeutic effects or dangerous bleeding complications, emphasizing the need for stringent monitoring and education regarding alcohol consumption in this demographic.
Moreover, the aging process itself dictates a decrease in physiological resilience, rendering older adults more susceptible to alcohol's effects. This vulnerability is compounded by the fact that the liver's efficiency in metabolizing substances diminishes with age, prolonging the half-life of both alcohol and certain medications in the bloodstream. Consequently, even moderate alcohol consumption can significantly augment the risk of adverse reactions. Additionally, the renal clearance of drugs is also compromised in the elderly, further complicating the safe management of medication in combination with alcohol. This scenario necessitates a comprehensive evaluation of an individual's medication regimen in conjunction with their alcohol intake to mitigate potential risks effectively.
Addressing the intricacies of alcohol and medication interactions within the older population not only involves meticulous clinical oversight but also requires dispelling prevalent myths about alcohol tolerance in seniors. It is imperative that healthcare providers engage in open dialogues with their patients, advocating for honesty regarding alcohol use. Educating older individuals about the potential hazards of mixing alcohol with their medications can prevent adverse events, enhance medication efficacy, and ultimately, safeguard their well-being. The table below outlines common interactions between alcohol and frequently prescribed medications in the elderly, highlighting the importance of awareness and preventive strategies.
| Medication Type | Common Interaction with Alcohol | Potential Effect on Older Adults |
|---|---|---|
| Cardiovascular medications (e.g., antihypertensives, warfarin) | Altered metabolism and increased risk of bleeding | Risk of hypertension, stroke, or serious bleeding events |
| Sedatives and hypnotics (e.g., benzodiazepines, sleep aids) | Enhanced sedative effect | Increased risk of falls, respiratory depression, cognitive decline |
| Analgesics (e.g., NSAIDs, opioids) | Increased risk of gastrointestinal bleeding, enhanced sedative effect | Higher likelihood of gastrointestinal issues, respiratory depression, addiction |
Addressing Misconceptions about Alcohol Tolerance in Seniors
A prevalent misconception exists suggesting that seniors can maintain the same alcohol tolerance levels as they did in their younger years. This belief, however, is fraught with misunderstanding about the physiological changes that accompany aging. As individuals age, their body composition undergoes significant alterations, notably a decrease in water content and lean body mass, alongside an increase in fat tissue. These transformations result in a reduced volume of distribution for alcohol, leading to higher concentrations of alcohol in the blood after consuming the same amounts as before. Consequently, the effects of alcohol are felt more swiftly and potently, elevating the risks of falls, cognitive impairment, and other alcohol-related complications.
Adding complexity to this issue is the declining metabolic efficiency in older adults. The liver, pivotal in detoxifying substances, operates at a diminished capacity with age, extending the period alcohol remains in the body and thereby intensifying its impact. This diminished metabolic function underscores the need for heightened caution regarding alcohol consumption among the elderly population. Compounded with potential interactions between alcohol and medications—common in older age—this necessitates a reevaluation of drinking habits as individuals advance in years.
Moreover, there exists a critical need for healthcare professionals to actively dispel these misconceptions through patient education. Highlighting the dangers associated with unchanged drinking patterns in the face of aging can guide more informed choices regarding alcohol usage. Educating seniors on the altered dynamics of alcohol tolerance is paramount in fostering safer drinking behaviors, thereby mitigating risks associated with alcohol consumption in this demographic.
In conclusion, the myth of unchanged alcohol tolerance in seniors is not only unfounded but also dangerous. An understanding of the physiological changes brought on by aging can aid in recognizing the increased vulnerabilities to alcohol's effects. Such awareness is crucial for both individuals and healthcare providers, driving towards tailored advice and interventions that cater to the unique needs of the older adult population. Addressing these misconceptions head-on will pave the way for healthier lifestyle choices and enhanced wellbeing among seniors.
By: Dr. Robyn Jordan